
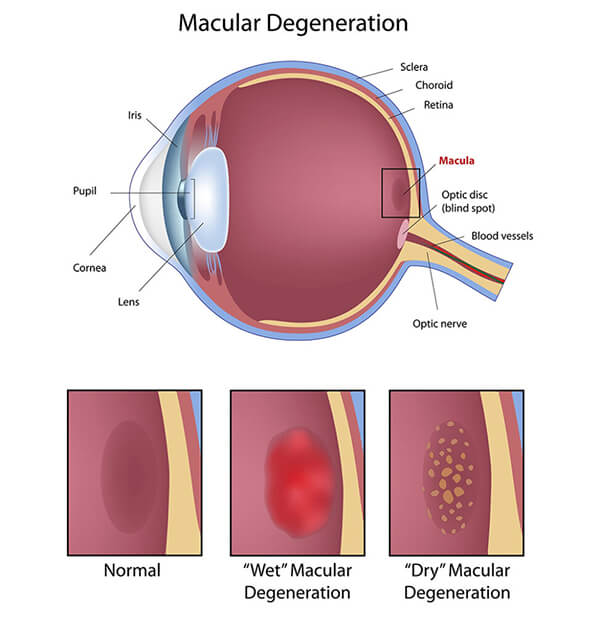
Age-related macular degeneration (AMD) is the leading cause of irreversible severe central vision loss in Caucasians 50 years and older in the United States.
AMD is a common eye disease associated with aging that gradually destroys sharp, central vision. Because side vision remains good, macular degeneration doesn’t cause total blindness.
The Progression of AMD can be slow or rapid, but the deterioration of central vision generally occurs over a period of a few years. So, if you experience the following, see your Eye M.D.:
Although it isn’t certain what causes macular degeneration, several studies have shown the following individuals may be at risk:
Laser treatment and intraocular medications (Avastin and Lucentis) can treat the “wet” form of macular degeneration (the rarer, but more severe form). However, there is no proven, effective treatment yet for the “dry” form (the most common form). But with both, low vision rehabilitation can help those with significant vision loss to maintain an excellent quality of life.
Studies to find effective treatments are ongoing, such as those that found high levels of zinc and antioxidants play a key role in slowing the progression of AMD. But as always, early detection is your best defense against losing vision. So if you are at risk, see your Eye M.D. for a complete eye exam at least every one to two years.
Vitamins and nutritional supplements have long been thought to play a role in slowing the progression of age-related macular degeneration. A study published in the October 2001, edition of Archives of Ophthalmology confirmed this theory. Patients with dry macular degeneration that received vitamin supplementation showed a 25% decrease in severe vision loss. The researchers also noted a 25% decrease in the progression to advanced macular degeneration. Antioxidants and zinc each showed a benefit, but a combination of the two was most effective. We believe that Lutein, which was not involved in this study, to be of significant benefit as well. Previous studies have shown beneficial effects with Lutein added to the diet of in-patients who have macular degeneration.
The vitamins used in this study included Vitamin C, Vitamin E, Betacarotene and Zinc, as well as Copper, which is necessary with Zinc supplementation to prevent anemia associated with high doses of Zinc. There are many formulations available over-the-counter and through health food stores as well as through mail order and on-line distributors.
In light of this data, we recommend nutritional supplementation in accordance with the above-mentioned study for patients with intermediate and advanced dry age-related macular degeneration. In addition, we recommend the use of an Amsler grid to monitor visual changes that may signal progression to the wet form of macular degeneration. Also noted is that Betacarotene supplementation is contraindicated in patients who smoke.
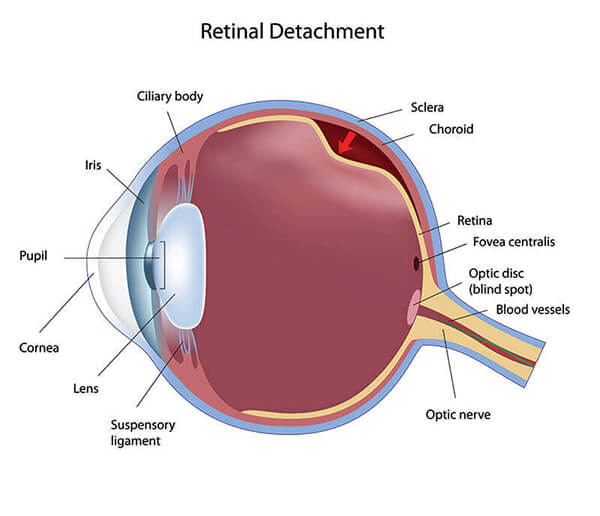
Retinal detachments are the separation of the retinal tissue from the inside wall of the eye. Similar to wallpaper coming loose from the wall, the retinal tissue may develop folds or come completely away from its proper position along the interior of the eye resulting in loss of vision.
Retinal tears involve a rip or tear in the tissue compromising the retina. They usually arise from a thinning or degenerative change in the peripheral retina. The retina is a layer of photoreceptor nerve cells lining the back of the eye and just like film in a camera, the retina reacts to the presence of light. These photoreceptor nerve cells generate an electrical impulse whenever they are exposed to light and these nerve impulses travel through the optic nerve to the brain where an image is perceived.
When the retina is torn, vitreous fluid (the inner gel fluid of the eye) is able to seep through the tear and accumulate behind the retina. This causes the retina to detach from the inside lining of the eye. Once a retinal detachment is started, it usually continues until most of the retina is completely separated from the interior of the eye resulting in blindness in the effected region.
Persons who have experienced a blow to the head or an injury to the eye are at risk for retinal tears and detachments. Nearsighted individuals are at a higher risk for retinal tears and detachments than other patients. The risk of spontaneous retinal tears and detachments increase slightly as we grow older.
Symptoms of retinal tears and detachments are new floaters, the sudden appearance of flashes of light in the vision, or a noted new occurrence of a shadow or curtain being pulled over a portion of the vision of one eye. Also, sudden decreased vision can be a symptom of a retinal tear or detachment.
Advances in surgical technology and techniques have resulted in a good success rate for repairs of retinal tears and detachments. The success of these surgical procedures is related to the size of the tear and the amount of detachment as well as the timeliness of the treatment. Surgery to repair retinal tears usually involves the use of lasers. These instruments are used to create a scar around the torn region that usually prevents the tear from progressing to a retinal detachment.
Tears flow along the edge of the eyelids toward the nose over the surface of the eye. Just before reaching the corner of the eye, the tears flow into two tiny drain tubes and then into a larger tube that carries the tears into the nasal passages. This explains why crying often causes the nose to become congested.
Several problems may cause the tear system to drain poorly. An accident may cut one or two of the tiny drain tubes or a long-standing infection may scar these tubes. Tumors, both malignant and non-malignant, may invade parts of the tear system and when the lacrimal drainage system becomes obstructed for any of these reasons, tears are unable to drain properly and tend to roll down the cheeks. Many times tearing is due to aging changes of the lid, such as laxity of the muscle of the lower lids or the misalignment of the tiny drain tubes called puncta. Therapy in the form of massage, warm compresses and medications are often effective, and in other cases surgical intervention is necessary to obtain relief of this tearing disorder.
Diabetes is a disease that occurs when the pancreas doesn’t secrete enough insulin or the body is unable to process the insulin and blood glucose properly. Diabetes can affect both children and adults.
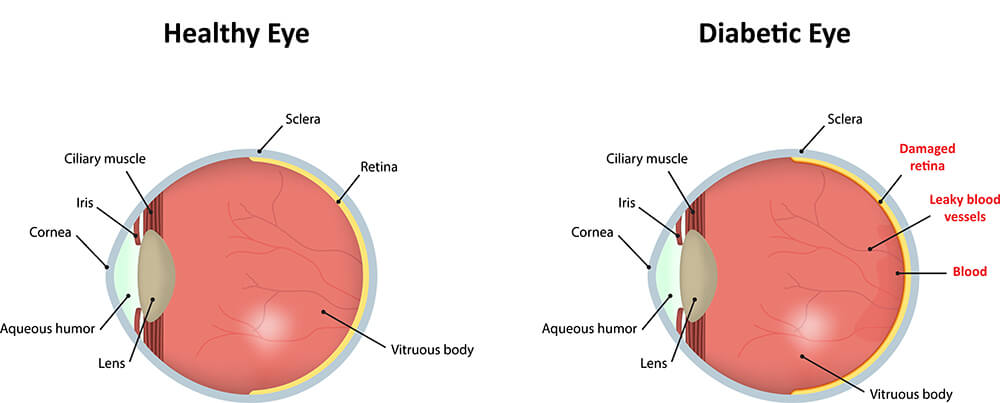
Patients with diabetes are more likely to develop eye problems such as cataracts and glaucoma but the disease’s effect on the retina is the main concern and threat to a person’s vision. Most diabetic patients develop eye changes that affect the retina approximately 20 years after their diagnosis of diabetes. The affect of diabetes on the retina of the eye is called diabetic retinopathy.
Over time diabetes affects the circulatory system of the retina with the earliest phase of the disease termed background or non-proliferative diabetic retinopathy. In this phase of diabetic retinopathy, arteries in the retina become weakened and may leak forming small “dot and blot” hemorrhages and cause swelling or edema of the retina with associated decreased vision.
The next stage or phase of diabetic retinopathy is termed proliferative diabetic retinopathy. In this stage, circulation problems cause areas of the retina to become oxygen deprived or what is termed aschemic. New, very fragile blood vessels begin to grow and develop. This process is called neovascularization. Unfortunately, these delicate vessels leak and hemorrhage quite easily causing hemorrhages into the vitreous gel of the eye and can cause associated decreased vision. Extensive proliferative retinopathy can lead to other serious problems such as retinal detachment.
The effect of diabetic retinopathy on vision varies widely depending on the stage of the disease. Some common symptoms of diabetic retinopathy include blurred vision, often linked to fluctuations in blood sugar levels; fluctuations, floaters, and flashes; or sudden loss of vision. Diabetic patients require routine eye examinations so that related eye problems can be detected and treated as early as possible. Most diabetic patients are frequently examined by an internist or endocrinologist who works closely with the ophthalmologist. A diagnosis of diabetic retinopathy is made following a detailed examination of the retina. Most patients with diabetic retinopathy can be helped if the diagnosis and treatment is early.
The treatment of diabetic retinopathy is multi-focal, including excellent regulation of the patient’s systemic diabetic status. Laser treatment (photocoagulation) is usually the treatment of choice for both proliferative diabetic retinopathy as well as some patients who have non-proliferative retinopathy with macular edema. With photocoagulation for the proliferative retinopathy, the surgeon uses a laser to destroy oxygen-deprived retinal tissue outside of the patient’s central vision. While this creates blind spots in the peripheral vision, this laser therapy prevents the continued growth of the fragile neovascularization and seals the leaking blood vessels. The goal of treatment is to arrest progression of the disease.
Vitrectomy is another surgical procedure commonly needed by diabetic patients who suffer a vitreous hemorrhage. During a vitrectomy, the surgeon carefully removes blood and vitreous from the eye and replaces it with a clear saline solution.
Patients with diabetes are at a greater risk of developing retinal tears and retinal detachment. Tears are often sealed with laser surgery. Retinal detachment requires surgical treatment to reattach the retina of the eye. The prognosis for visual recovery is variable and dependent on the severity of the retinal detachment.
Ophthalmology & Retina Associates of Georgia LLC
5185 Peachtree Parkway, Suite 365,
Phone: 404-777-2020
Fax: 404-777-7701